In today’s digital age, telemedicine apps have become an integral part of the healthcare industry. With the ability to connect doctors and patients remotely, these apps provide convenience, efficiency, and accessibility to medical assistance. However, one question that often arises is the cost of developing a telemedicine app. In this article, we will delve deep into the factors that influence the cost of telemedicine app development and provide valuable insights for CTOs, founders, and tech leaders looking to venture into this sector.
What is a Telemedicine App?
The definition of a Telemedicine App
A telemedicine app is a platform that enables healthcare professionals and patients to communicate and exchange medical information remotely. Through the use of video consultations, in-app chats, and other features, these apps bridge the physical gap between doctors and patients, making healthcare services more readily available.
Telemedicine apps have revolutionized the way healthcare is delivered. In the past, patients had to travel long distances to see a specialist or wait for hours in crowded waiting rooms. With telemedicine apps, patients can now connect with doctors from the comfort of their own homes, eliminating the need for unnecessary travel and reducing the risk of exposure to contagious diseases.
These apps are designed to be user-friendly and accessible to people of all ages and technological abilities. They often have intuitive interfaces that allow patients to easily navigate through different features, such as scheduling appointments, uploading medical records, and communicating with healthcare professionals.
The Importance of Telemedicine Apps in Healthcare
The significance of telemedicine apps in the healthcare industry cannot be overstated. These apps offer numerous benefits to both doctors and patients. For doctors, telemedicine apps allow them to expand their reach beyond geographical boundaries, provide remote consultations, and manage appointments more efficiently.
With telemedicine apps, doctors can now reach patients in remote areas where access to healthcare services may be limited. This is particularly beneficial for individuals living in rural communities or areas with a shortage of medical professionals. By leveraging telemedicine apps, doctors can provide timely medical advice, monitor chronic conditions, and even prescribe medications without the need for in-person visits.
On the other hand, patients can easily access doctors, schedule appointments without long waiting times, and receive medical advice from the comfort of their homes. Telemedicine apps empower patients to take control of their healthcare by providing them with convenient and timely access to healthcare professionals. This can be especially beneficial for individuals with mobility issues, elderly patients, or those with busy schedules.
Moreover, telemedicine apps have the potential to reduce healthcare costs for both patients and healthcare providers. By eliminating the need for unnecessary hospital visits or emergency room trips, telemedicine apps can help reduce healthcare expenses. Additionally, telemedicine consultations are often more affordable compared to in-person visits, making healthcare more accessible and affordable for a wider population.
Furthermore, telemedicine apps have proven to be instrumental during public health crises, such as the COVID-19 pandemic. These apps have played a crucial role in reducing the spread of the virus by enabling healthcare professionals to provide virtual consultations and triage patients remotely. By minimizing in-person interactions, telemedicine apps have helped to protect both patients and healthcare workers from potential exposure to the virus.
In conclusion, telemedicine apps have revolutionized the healthcare industry by bridging the gap between doctors and patients, improving access to healthcare services, and reducing healthcare costs. With the advancements in technology, telemedicine apps will continue to play a vital role in shaping the future of healthcare delivery.
Key Features of a Telemedicine App
Now that we have a basic understanding of telemedicine apps, let’s explore the key features that make these apps truly exceptional.
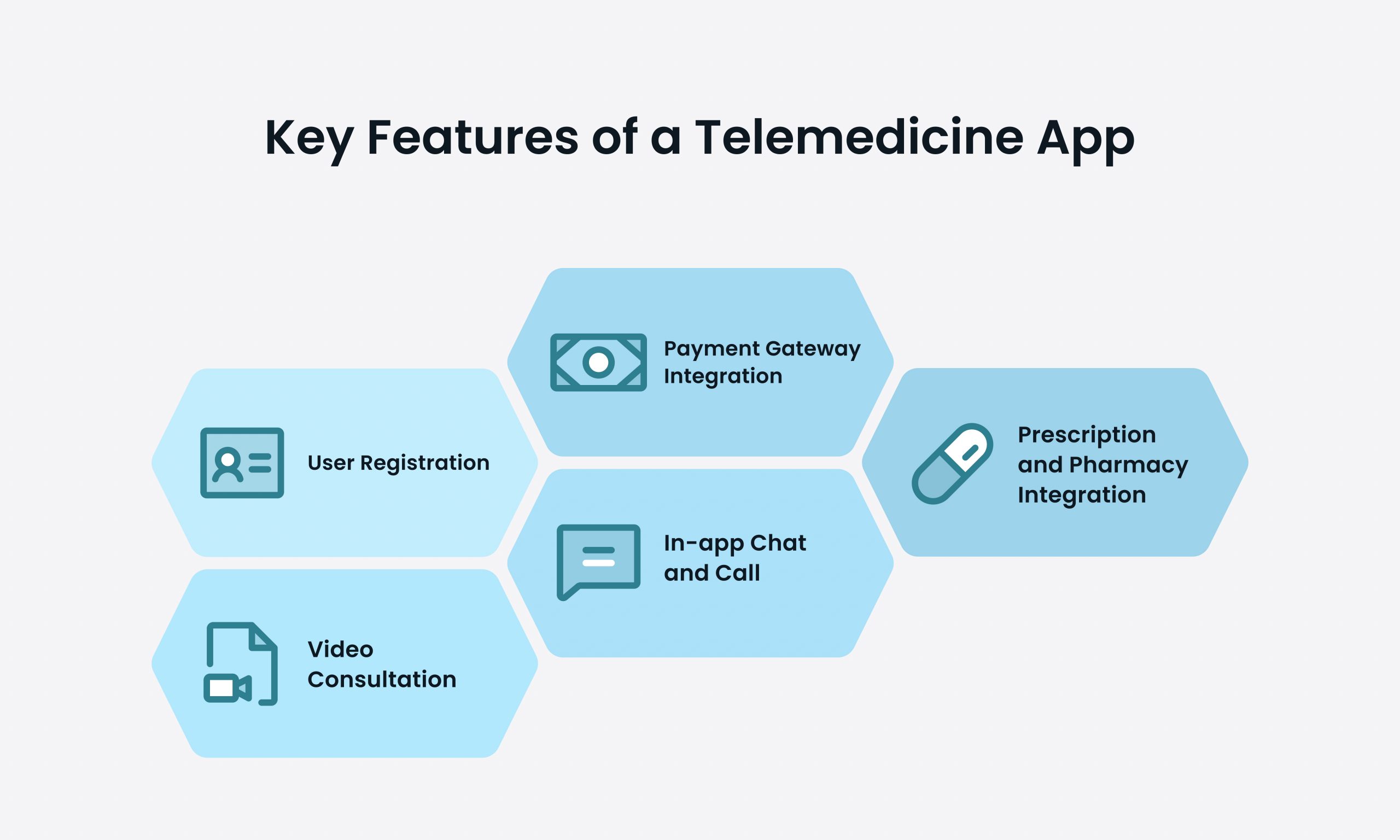
User Registration
One of the primary features of a telemedicine app is user registration. This allows patients to create accounts and provide relevant information, such as their medical history, allergies, and demographic details. User registration ensures that doctors have access to the necessary information to provide accurate consultations and personalized care.
When patients register on a telemedicine app, they are prompted to fill out a detailed form that captures their medical history. This includes information about previous diagnoses, surgeries, medications, and allergies. Additionally, patients can provide their demographic details, such as age, gender, and location. This comprehensive registration process ensures that doctors have a holistic view of the patient’s health and can make informed decisions during consultations.
Furthermore, user registration also allows patients to set their preferences and customize their experience on the app. They can choose their preferred language, set notification preferences, and even select their preferred doctors or specialists. This personalization feature enhances the user experience and ensures that patients feel comfortable and in control of their healthcare journey.
Video Consultation
Video consultation is the backbone of any telemedicine app. It enables doctors and patients to connect face-to-face remotely. During a video consultation, doctors can visually assess patients, discuss symptoms, provide diagnoses, and prescribe medications or advice. The video consultation feature requires reliable and secure technology to ensure the privacy and confidentiality of patient information.
When patients initiate a video consultation, they are connected to a virtual waiting room where they can relax and prepare for their appointment. The app notifies them when the doctor is ready, and they can seamlessly join the video call. The video consultation interface is designed to mimic an in-person consultation, with features like the ability to share medical reports or images, and a chatbox for real-time communication.
Telemedicine apps also incorporate advanced features to enhance the video consultation experience. For example, some apps allow doctors to annotate on the patient’s screen, making it easier to explain medical conditions or treatment plans. Other apps offer translation services, enabling doctors and patients to communicate effectively, even if they speak different languages. These additional features make telemedicine apps more versatile and accommodating for diverse patient populations.
Prescription and Pharmacy Integration
Integration with prescription and pharmacy services streamlines the process of prescribing and delivering medications to patients. By integrating with pharmacy services, telemedicine apps can automate the prescription process, making it faster, more accurate, and reducing the chances of errors. Patients can conveniently order medications through the app and have them delivered to their doorstep.
When doctors prescribe medications through a telemedicine app, the prescription is automatically sent to the integrated pharmacy. The pharmacy receives the prescription, prepares the medication, and arranges for its delivery. This integration eliminates the need for patients to physically visit a pharmacy, saving them time and effort.
Furthermore, telemedicine apps often provide medication reminders and alerts to ensure that patients adhere to their prescribed treatment plans. These reminders can be customized based on the medication schedule, dosage, and frequency. By integrating prescription and pharmacy services, telemedicine apps empower patients to manage their medications effectively and improve their overall health outcomes.
In-app Chat and Call
In addition to video consultations, telemedicine apps often offer in-app chat and call options. These features allow doctors and patients to communicate in real-time, exchange messages, and seek clarifications. The in-app chat and call features are particularly useful for non-urgent queries, follow-ups, or for patients who may face connectivity issues for video consultations.
Patients can initiate an in-app chat or call with their doctors at any time. This feature enables them to ask questions, provide updates on their condition, or discuss any concerns they may have. Doctors can respond to these messages or calls at their convenience, ensuring that patients receive timely responses and support.
In-app chat and call features also facilitate collaboration between doctors and patients. For example, doctors can share educational resources, articles, or videos with patients to help them understand their condition better. Patients can also upload images or reports through the chat feature, allowing doctors to review them and provide informed guidance.
Payment Gateway Integration
To ensure a seamless user experience, telemedicine apps often integrate with payment gateways. This allows patients to easily pay for consultations, prescriptions, or other services within the app. Integration with popular payment systems ensures secure transactions and enhances the overall user experience.
When patients need to make a payment on a telemedicine app, they can choose from various payment options, such as credit cards, debit cards, or digital wallets. The app securely processes the payment and provides a digital receipt for the transaction. Patients can view their payment history within the app and easily track their healthcare expenses.
Integration with payment gateways also enables telemedicine apps to offer flexible pricing models. Some apps allow patients to pay per consultation, while others offer subscription plans for unlimited access to healthcare services. This variety of payment options ensures that telemedicine remains accessible to patients with different financial capabilities.
In conclusion, telemedicine apps offer a range of features that revolutionize the way healthcare is delivered. From user registration and video consultations to prescription integration and in-app communication, these apps provide convenience, accessibility, and personalized care to patients. Through continuous advancements in technology, telemedicine apps are transforming the healthcare landscape and improving patient outcomes.
Factors Influencing the Cost of Telemedicine App Development
Now that we have explored the key features of a telemedicine app, let’s dive into the factors that influence the cost of developing such an app.
App Complexity and Features
The complexity and number of features included in a telemedicine app significantly impact the telemedicine app development cost. Advanced features like AI-powered symptom analysis, integration with wearable devices, or electronic health record (EHR) integration require a higher level of expertise and development time, thus increasing the cost of development.
Design and User Interface
A well-designed and intuitive user interface is crucial for the success of any mobile app, including telemedicine apps. Investing in a visually appealing design, seamless navigation, and user-friendly interface is important to ensure a positive user experience. However, high-quality design and UI/UX expertise can also add to the overall telemedicine app development cost.
Platform Selection (iOS, Android, or Both)
The choice of platforms, whether iOS, Android, or both, impacts the telemedicine app development cost. Developing an app for a single platform is generally less costly compared to building for multiple platforms simultaneously. However, it’s important to consider the target audience and market share when deciding on platform selection.
Location and Size of the Development Team
The location and size of the development team play a role in determining the cost of telemedicine app development. Development rates vary across different regions due to differences in labor costs. Additionally, the size of the development team required to execute the project efficiently also affects the cost.
Post-Launch Support and Maintenance
Launch of the telemedicine app is just the beginning of the journey. Post-launch support and maintenance are crucial for ensuring the app’s smooth operation, bug fixing, and implementing new features or updates. As a software development company with proven expertise, WeSoftYou emphasizes the importance of investing in post-launch support to ensure a seamless experience for users.
From our experience at WeSoftYou, the cost of developing a telemedicine app can range anywhere from $50,000 to $150,000 and beyond, depending on the complexity and scope of the project. It’s important to engage with a reputable software development company that understands the nuances of telemedicine app development and can provide accurate cost estimates based on your specific requirements.
Conclusion
Telemedicine apps have revolutionized the healthcare industry by bringing doctors and patients closer, virtually. The cost of developing a telemedicine app depends on various factors, including the complexity of the app, its features, design, platform selection, and post-launch support. WeSoftYou, with its expertise in software development, understands the intricacies of telemedicine app development and can guide you through the entire process.
FAQ
The development time for a telemedicine app varies based on the complexity and scope of the project. On average, it can take around 4 to 9 months from concept to launch.
Yes, it is possible to integrate an existing EHR system with a telemedicine app. This integration allows seamless access to patient records, improves the quality of care, and enhances overall efficiency.
Ensuring the security and privacy of patient data involves several crucial measures. This includes data encryption for both transit and storage, strict access controls with multi-factor authentication, regular auditing of access logs, comprehensive staff training, a secure IT infrastructure, diligent vendor assessment, data minimization, defined data retention policies, secure communication channels, a well-prepared incident response plan, adherence to regulatory standards, attention to physical security, continuous staff training on cybersecurity, and data segmentation based on sensitivity. By implementing these practices, a robust framework for safeguarding patient data can be established, reducing the risk of breaches and maintaining the confidentiality of sensitive information.






















